Your Trusted Partner in Billing & Practice Management Solutions
HealthPath Solutions offers expert medical/dental billing services with practice management solutions tailored for individual and group practices. We streamline your processes to enhance cash flow and reduce operational burdens for all specialties.
Get Started
Our Comprehensive Services
Services
Why Outsource
Why Outsource Your Medical Billing?
Increased Efficiency
Our expert team processes claims quickly and accurately, reducing denials and speeding up payments. Typically increasing revenue up to 30% or greater.
Cost Savings
Outsource to avoid hiring extra staff or investing in costly software—only pay for results with our performance-based fees.
Focus on Patient Care
Free up time and resources to focus on treating patients, while we handle the billing and collections.

What’s Our Process
Process
Consultation
We assess your practice’s needs to tailor our services to your goals.
Planning
We create a customized plan with clear strategies and timelines for success.
Implementation
Our team integrates billing tools and systems smoothly with minimal disruption.
Support
We provide ongoing support, regular monitoring, and performance reports to keep you informed.
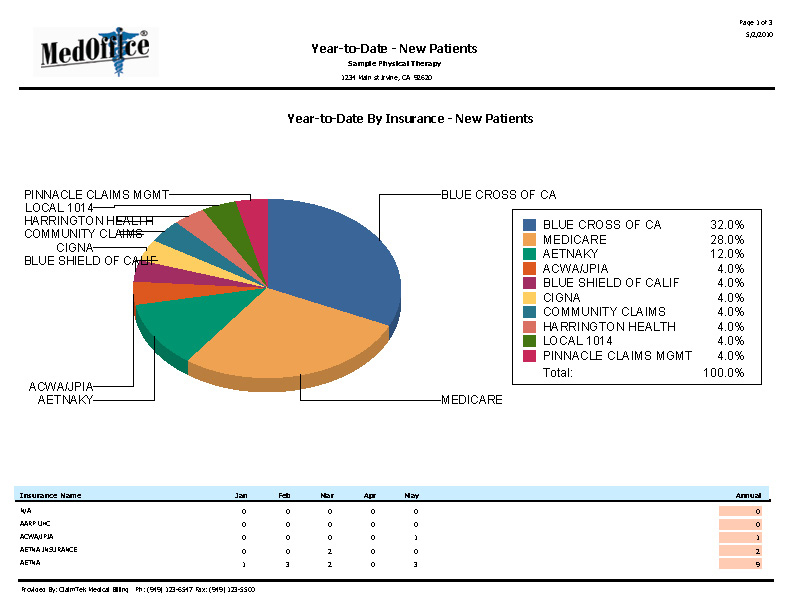
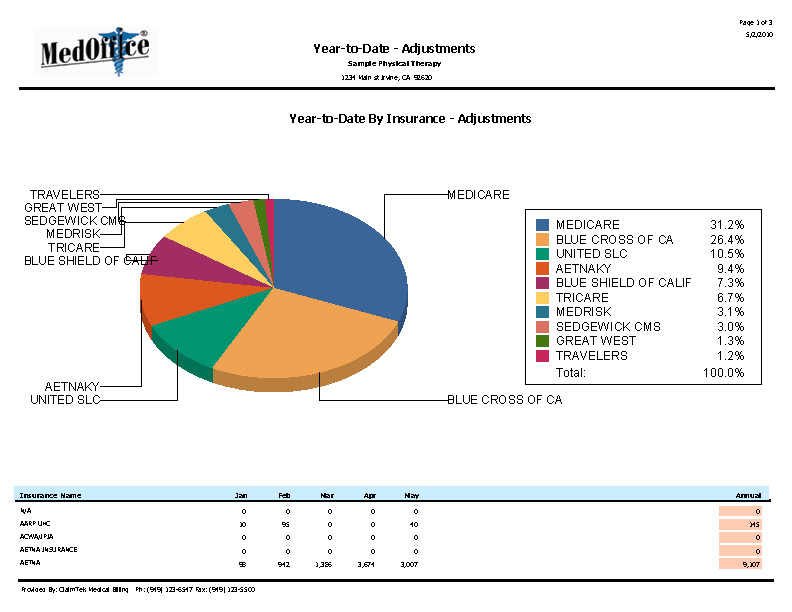
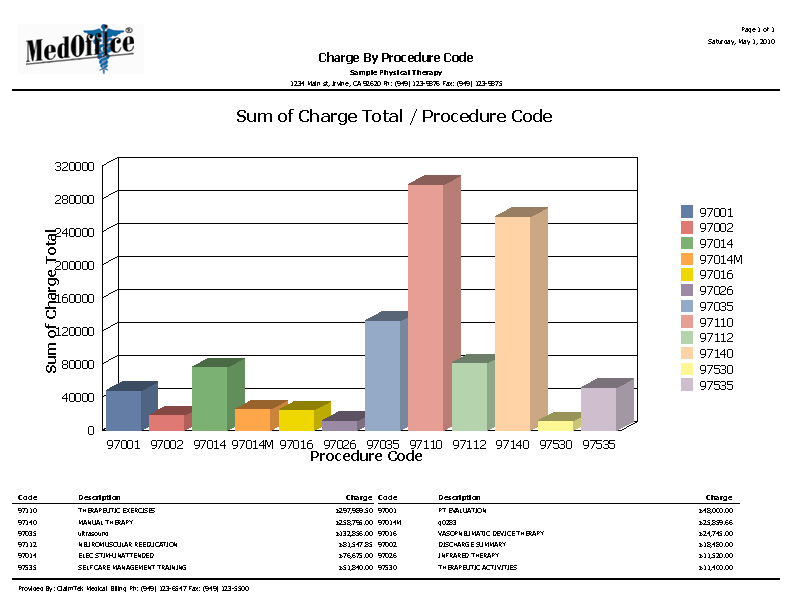
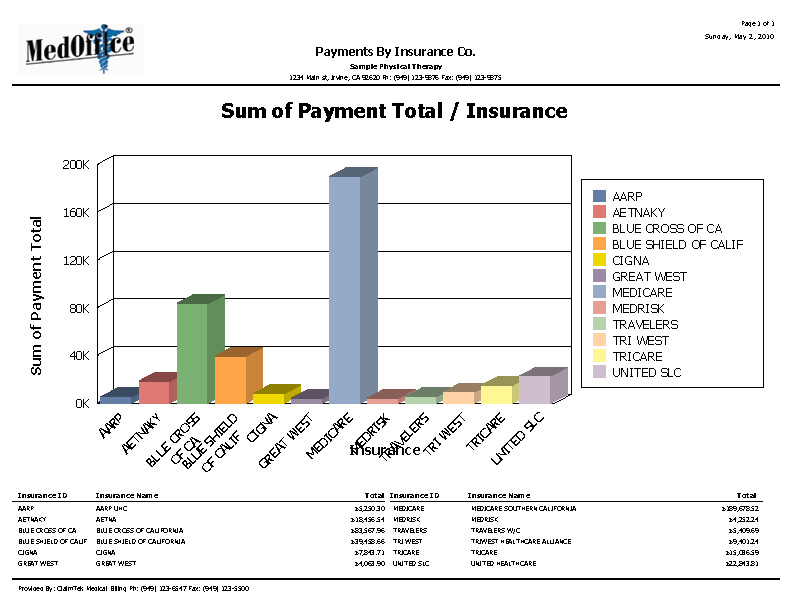
Report Analysis
Code & Cost Analysis
Get a clear view of your practice’s financial health with our detailed code and cost analysis reports. We provide in-depth insights that other services might overlook, helping you optimize billing and improve profitability.
Explore the comprehensive reporting structures we offer and see how our reports can make a difference for your practice.
We prefer to bill our own patient’s, but we’re interested in obtaining insurance claim processing services from you. Does your company offer this service?
We sure do!
Please keep in mind however, patient billing is best performed by your biller, who already has access to all account balances and other additional information. If we are already handling the insurance end of things, it makes sense to let our system automatically generate the claims on an as needed basis! We can provide you with our Remote Access/Viewing software, updated regularly, for an additional fee.
Remote Access enables your staff to view patient balances and generate their own statements, among many other things.
How do you handle non-payments from a patient?
We will send out no more than four statements, and make follow up phone calls. After 120 days we recommend that the account be turned over to collection and that the patient be denied future treatments until their account has been paid. If you are not already affiliated with a collection agency near you, please let us know.
We strongly recommend that an additional fee be applied to each account which has not received a payment within a 30 day period.
How do you handle non-payments from an insurance carrier? (denials, etc.)
We must first determine if the denial, whether in part or in full, is valid. If the denial is valid it must be written off. If the denial is not valid, as in many of the cases, we will request that the carrier reprocess the claim. Unfortunately, some carriers may require the claim to be resubmitted on paper via snail mail, additional charges may be invoiced to your account as a result.
How often will our patients be billed?
Any patient in our system will receive a bill for any balance due, once a payment has been received by their insurance carrier, if you have contracted for this service. Patients are billed bi-monthly. Payment Plans can be easily accommodated also.
How do we report payments received from our patients, for both co-payments and patient billing?
You can easily report a patient’s co-payment, made at the time of service, on their Superbill (Treatment form) for that day’s treatments.
You can also report all of the patient’s payments, received in the mail or electronically, by keeping a Payment Log. A payment log enables you to report all payments received in your office, using one simple form. If you do not already use this type of form in your practice, we can custom design one for you. You can also report all of the patient’s payments, received in the mail by making a copy of the check and attaching it to their patient statement remittance (if returned).